Breaking the Silence: Why Men’s Mental Health Deserves More Attention

Every day, millions of men carry silent battles behind composed faces.
They go to work. They show up for their families. They crack jokes with their friends. But underneath it all, many are quietly wrestling with anxiety, depression, loneliness, or burnout and far too often, they do it alone.
June is Men’s Mental Health Month, a time to spotlight a reality that often goes unspoken. For decades, the conversation around mental health has expanded, yet men remain one of the most underserved and overlooked groups in this space. Whether it’s due to stigma, cultural expectations, or lack of access, the truth is clear: men are hurting, and many don’t know where to turn.
This isn’t just about individual well-being. It’s about the ripple effects on families, workplaces, communities, and future generations. When men are denied the tools or permission to take care of their mental health, everyone feels the consequences.
This article is a call to awareness, but also to hope. We’ll explore the hidden crisis, the barriers men face, and most importantly, the paths to healing whether that starts in a therapist’s office, a text conversation, or a quiet moment of self-reflection.
Because every man deserves more than survival. He deserves support. He deserves care. He deserves to feel like he’s not in this alone.
The Silent Epidemic
Men are struggling, and far too often, they're doing it in silence.
While society has made progress in opening up conversations about mental health, one group consistently remains overlooked: men. The cost of that silence is devastating.
Breaking the Silence: Why Men Need to Talk About Their Mental Health | Henry Nelson Case | TEDxAUBG
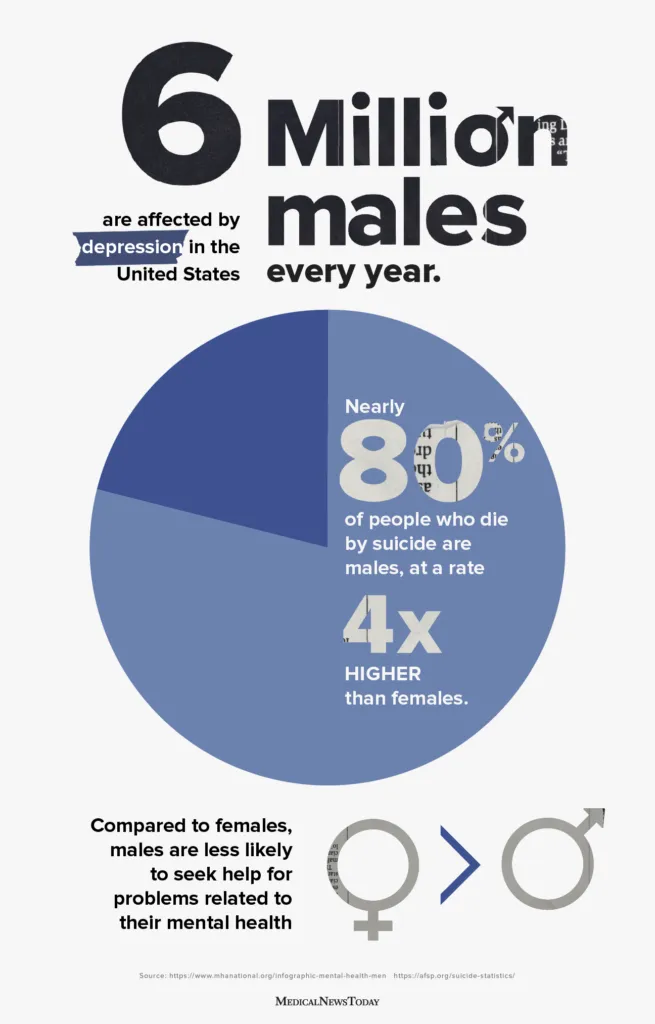
According to the World Health Organization, men die by suicide nearly twice as often as women globally. In the United States, that number is even more alarming. Men account for nearly 80 percent of all suicides. Depression, anxiety, PTSD, and substance abuse affect men just as deeply, yet they are far less likely to be diagnosed or treated.
Why? Because most men were never taught how to talk about what they feel.
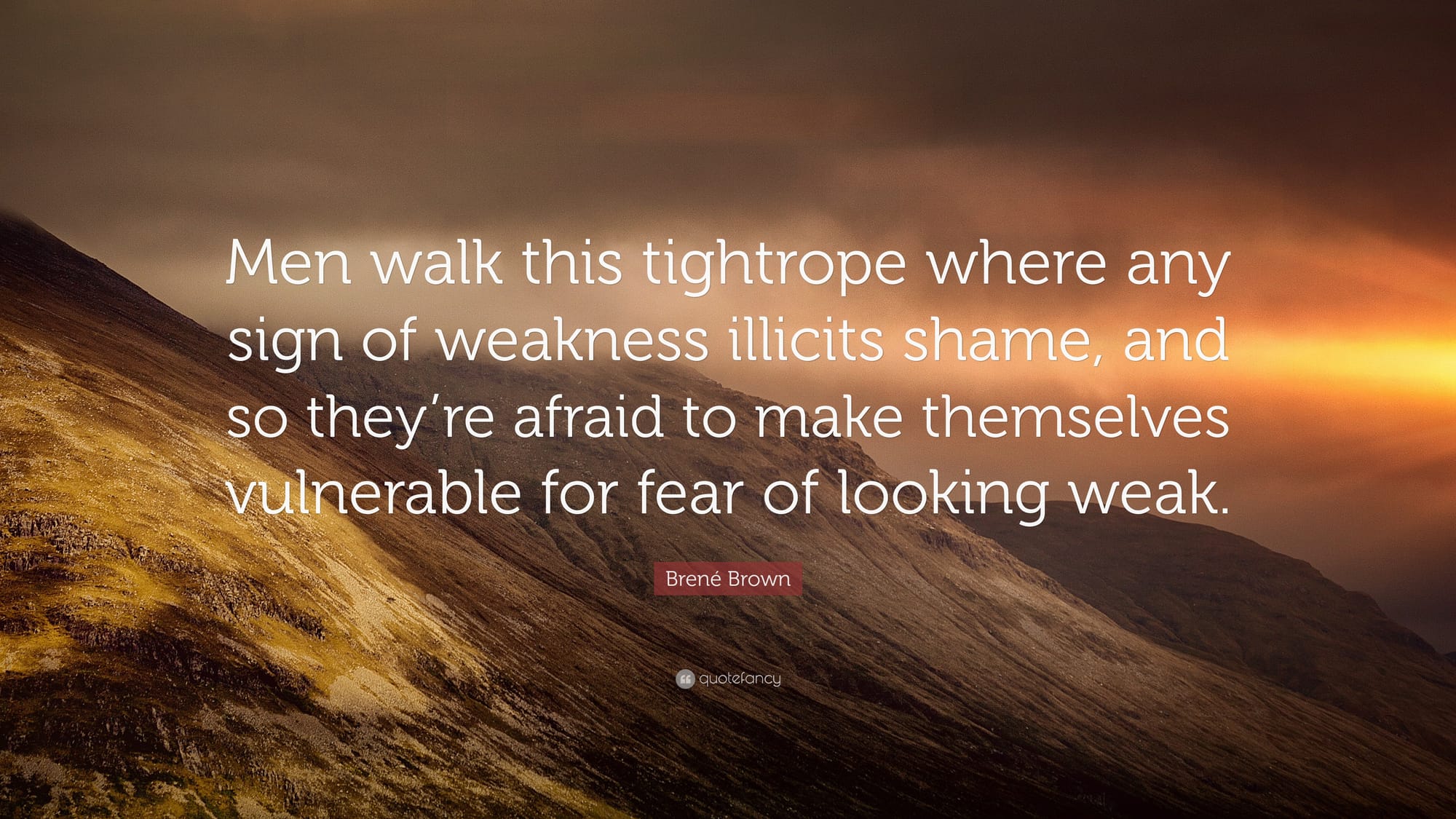
From a young age, many boys absorb an unspoken rulebook. Don’t cry. Be tough. Handle it yourself. Emotional pain is seen as weakness, and asking for help is viewed as failure. These beliefs don’t just shape personalities, they shape outcomes. Boys grow into men who believe their emotional struggles are something to endure alone, not something to heal.
The problem doesn’t end with gender. If you're a Black man, an immigrant, an Indigenous father, a gay teen, or a working-class veteran, the pressure to stay silent is often intensified by racism, discrimination, homophobia, or financial stress. The mental health system, often designed with a narrow perspective, is not always equipped to support these men in ways that reflect their lived experiences.
These statistics are not just numbers. They represent fathers, sons, brothers, and friends. Behind every one of them is a life that might have taken a different turn if seeking help had felt a little more acceptable and support had been a little more accessible.
This is the silent epidemic. But it can be named. It can be faced. And it can be changed.

Barriers to Mental Health Support
Even when men recognize that something is wrong, many still don’t reach out for help. The reasons are layered, and the barriers are everywhere.
The first is stigma. Mental health struggles are still seen by many men as a sign of weakness. In cultures where strength and control are closely tied to masculinity, admitting to anxiety, depression, or trauma can feel like admitting failure. Many men would rather push through silently than risk being judged, misunderstood, or seen as broken.
Then there is the emotional language gap. Decades of conditioning often leave men without the vocabulary to explain what they are feeling. Instead of saying “I’m feeling overwhelmed,” a man might say, “I’m just tired” or “I’m fine” even when he is not. Emotional discomfort gets bottled up, and in time, it shows up in other forms—irritability, substance use, physical health issues, or isolation.
Practical access is another obstacle. Many men work long hours or juggle multiple responsibilities. Taking time off for therapy can feel unrealistic, especially in work environments that don’t support mental health care or offer paid time off. For some, therapy is simply unaffordable. For others, it feels intimidating or irrelevant especially if they have never seen anyone like them talk openly about getting help.
Cultural factors can make it even harder. In some communities, mental health is still considered taboo. In others, therapy is seen as a luxury for the privileged. Older generations may believe that suffering in silence is the norm. Religious or traditional values can sometimes discourage speaking to outsiders about personal matters.
And then there is the internal barrier. Many men convince themselves they are not “sick enough” to need support. They believe others have it worse. They downplay what they are going through because no one ever told them that emotional pain deserves care too.
The result is a system where men are less likely to ask for help and more likely to suffer longer before they do. Not because they are unwilling, but because the path to help has been made narrow, confusing, and full of shame.
Recognizing these barriers is the first step to removing them.
What Healing Can Look Like
Healing doesn’t always begin with a diagnosis. Sometimes, it starts with one honest conversation.
When men begin to open up whether with a friend, a partner, a therapist, or even a journal it often feels unfamiliar at first. Vulnerability can be uncomfortable. But time and time again, men who take that step report the same thing: relief. Not because everything is suddenly fixed, but because they no longer feel alone.
Therapy is one of the most effective tools available. It provides a private space where men can say things they’ve never said before, explore where their pain comes from, and learn how to manage it without shame. There are different types of therapy, and not every style works for everyone. Some benefit from structured approaches like Cognitive Behavioral Therapy (CBT), while others prefer more open, conversational models.
Medication can also play a role, especially for conditions like depression, anxiety, or PTSD. For many, it reduces the intensity of symptoms enough to allow other forms of healing to begin. It’s not about changing who you are. It’s about clearing the fog so you can move forward.
But healing doesn’t only happen in professional settings. Men’s groups, online communities, and peer-led support circles are growing around the world. These spaces help break isolation by allowing men to talk openly with others who understand. The power of being seen and heard without judgment can be transformative.
Even small habits can make a big difference. Exercise, mindfulness, spending time in nature, journaling, reducing alcohol, and improving sleep are not replacements for therapy, but they are powerful allies. Healing is not a straight line, and it doesn’t look the same for everyone. But the key is movement choosing care over suppression, connection over isolation.
Technology is also creating new ways to begin. AI tools like Aitherapy offer an accessible starting point for men who aren’t ready to talk to someone in person. With 24/7 availability and total privacy, tools like this can help men start sorting through their thoughts and emotions at their own pace. It’s not meant to replace therapy, but it can be a first step toward it.
What matters most is this: healing is possible. You don’t have to stay stuck. You don’t have to stay silent. And you don’t have to do it alone.
What You Can Do
The conversation around men’s mental health can’t just be theoretical. Real change starts with action both for ourselves and for the people we care about.
If you're struggling
You don’t need to have a breakdown to deserve support. If you're feeling numb, irritable, anxious, disconnected, or just not like yourself, those are valid reasons to get help. Here are a few steps you can take:
- Talk to someone you trust. This could be a friend, a partner, a family member, or a professional. You don’t have to have the perfect words—just start with honesty.
- Try journaling. Writing things down can help you process emotions you might not even realize you’re carrying.
- Look into therapy. There are in-person options, online platforms, and affordable services depending on your needs. You don’t need a “serious” problem to go.
- Start small. Taking a walk, cutting back on drinking, or going to bed earlier may seem minor, but they can shift your mental state more than you think.
- Explore anonymous or AI tools. If you're not ready to open up to someone directly, Aitherapy or other private platforms can help you begin at your own pace.
If you love someone who is struggling
Men don’t always show they’re hurting in obvious ways. It may look like anger, silence, workaholism, or withdrawal. If you notice something off in someone you care about:
- Check in regularly. A simple “How have you been feeling lately?” can open a door.
- Don’t push, just listen. Many men won’t open up if they feel interrogated or judged. Listen without fixing.
- Normalize help. Share stories of others who’ve gone to therapy or used support tools. Help them see it as strength, not weakness.
- Model vulnerability. Being open about your own struggles gives others permission to do the same.
- Stay patient. Healing is a process. Just being there can make a bigger impact than you think.
In your community or workplace
The stigma around men’s mental health won’t disappear unless we challenge it where we live and work. Here’s how:
- Speak up. If you’re in a leadership position, talk about mental health openly and make resources visible.
- Support time off for mental wellness. Encourage rest, boundaries, and recovery as part of a healthy culture.
- Promote diverse resources. Mental health is not one-size-fits-all. Make sure different identities and needs are represented.
- Support campaigns. Organizations like Movember, The ManKind Project, and Mental Health America are doing powerful work during this month and beyond. Contributing your time, money, or platform helps keep the momentum going.

It’s Time to Change the Story
For too long, men’s mental health has been treated like a footnote in the larger conversation about wellbeing. But it’s not a side issue. It’s a crisis hiding in plain sight one that touches every community, every family, and every generation.
Men are taught to carry the weight without asking for help. They’re praised for being strong, but not for being honest. They’re expected to stay calm, even when everything inside them is unraveling. This model of masculinity is not just outdated, it’s dangerous.
But the good news is, change is already happening. More men are stepping forward and saying, “I need support.” More workplaces are opening up space for mental health. More tools, like online therapy and AI companions, are making help easier to reach. Slowly, the silence is being broken.
If you’re a man reading this and you’ve been struggling, know that you’re not alone. You don’t have to wait until things fall apart to deserve care. Whether you speak to a friend, call a therapist, or try a tool like Aitherapy, what matters is taking the first step. Healing begins with honesty.
If you love a man who seems distant, angry, or numb—reach out. Not with pressure or solutions, but with presence. Sometimes knowing that someone sees you is enough to start a shift.
Men’s Mental Health Month isn’t just about raising awareness. It’s about rewriting the script. One where strength includes softness. One where asking for help is respected. One where silence doesn’t win.
Let’s not wait for another headline or statistic. Let’s make care the norm, not the exception.
Have you talked with Aitherapy yet?